Most physicians in entrepreneurial medicine practices manage patients in perimenopause and menopause. Updated guidelines and newer data now challenge the conclusions that shaped hormone therapy decisions for two decades.
At Private Physicians Alliance’s most recent annual meeting, Dr. Bojana Jankovic Weatherly and Dr. Shamita Trivedi presented updated guidelines on menopausal hormone therapy. Their session covered hormonal and non-hormonal options, risk stratification strategies, and the integrative approaches that round out a complete treatment plan.
Where the WHI Got It Wrong
The Women’s Health Initiative reshaped hormone therapy prescribing in 2002. Up to 40% of postmenopausal women were prescribed hormone therapy before the study. Today, that number sits around 5%.
The WHI included women aged 50–79. The average age was 63. Many were smokers. Many were obese. These women received oral conjugated equine estrogens and medroxyprogesterone, formulations that are no longer first-line therapy.
When researchers examined the 50-to-59 subgroup separately, none of the findings reached statistical significance. The subset analysis wasn’t powered to draw conclusions about women starting therapy around the menopausal transition.
“Maybe there are some trends here, but we really don’t know for sure,” Dr. Weatherly noted. “And these are oral formulations that don’t reflect what we typically start with today.”
Current Indications and Prescribing Principles
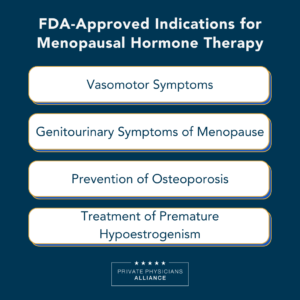
The FDA approves menopausal hormone therapy for four indications: vasomotor symptoms, genitourinary symptoms of menopause, prevention of osteoporosis, and treatment of premature hypoestrogenism.
The 10-year window matters. Starting hormone therapy within 10 years of menopause and under age 60 is where the data supports a lower risk relative to benefit for most women.
This doesn’t mean a rigid cutoff at 60. A small 2024 study showed no strokes or MIs when therapy continued beyond 65 in a carefully selected cohort. The sample size limits conclusions, but it opens the door to individualized decisions with appropriate screening.
“There’s no one-size-fits-all,” Dr. Trivedi said. “There’s no dose appropriate for everyone. It’s really okay to do trial and error with respect to formulations and dosing.”

Formulations and Delivery Methods
Transdermal estrogen is the starting point for most patients. Options include patches, gels, sprays, and emulsions.
Oral micronized progesterone provides uterine protection in women with a uterus. Some patients report grogginess or anxiety with oral progesterone. For these patients, vaginal administration of the same capsule or a compounded suppository offers an alternative. Data supports adequate uterine protection with vaginal delivery.
A progestin IUD can work for women who struggle with oral or vaginal progesterone and need uterine protection. This is off-label but backed by sufficient data.
“Bioidentical” is a marketing term. These hormones are biochemically identical to what the body produces, but they’re still synthesized in a lab from wild yams or soy. FDA-approved bioidentical options exist. Compounding has a role when a patient has a peanut allergy (Prometrium contains peanut oil), needs in-between dosing, or requires low-dose testosterone.
Risk Stratification in Practice
Breast cancer risk depends on what you prescribe and for how long.
Oral micronized progesterone used for up to five years does not appear to increase breast cancer risk. Synthetic progestins do increase risk. Use beyond five years with either option results in a small increase: approximately one per 1,000 women per year of use.
“Compare that to the risk of sedentary lifestyle, obesity, [and] alcohol use,” Dr. Weatherly said. “We have to take all of this in context.”
Venous thromboembolism risk is clear. Oral estrogen increases clotting risk. Transdermal estrogen and oral micronized progesterone do not. For patients with VTE concerns, transdermal is the obvious choice.
The timing hypothesis suggests that menopausal hormone therapy may reduce cardiovascular risk when started before age 60 or within 10 years of menopause. Subgroup analysis from a Cochrane review of 40,000 women showed 30% lower mortality and nearly 50% lower coronary heart disease risk in this population. The American Heart Association acknowledges these findings.
Starting therapy in women over 60 or more than 10 years post-menopause shows no cardiovascular benefit and a higher stroke risk. Estrogen appears to act differently depending on whether arteries have accumulated plaque and inflammation during years of estrogen deprivation.
The same timing window may matter for brain health. Women face twice the lifetime risk of developing Alzheimer’s compared to men. Early data suggests MHT initiated before age 60 and within 10 years of menopause may reduce age-related cognitive decline.
Studies are ongoing, but the pattern aligns with what we see in cardiovascular outcomes.
Beyond Hormones
Some patients have contraindications to estrogen. Others prefer non-hormonal options.
SSRIs, SNRIs, and gabapentin can address vasomotor symptoms. Veozah (fezolinetant), approved in 2023, offers another option. Dr. Trivedi typically starts with an SSRI, SNRI, or Veozah when considering non-hormonal pharmacotherapy.
Integrative approaches have data behind them. Specific yoga poses activate the parasympathetic nervous system: legs-up-the-wall, reclining butterfly, and wide-legged forward fold. These help with anxiety, fatigue, and insomnia. Dr. Trivedi, a certified yoga teacher, can point interested physicians to published trials on PubMed.
Mindfulness meditation supports real-time symptom management. Two minutes nightly for five days can produce noticeable results. It won’t replace hormone therapy, but it adds value for patients who want a complete approach.
Starting the Conversation
Fear from the WHI still shapes patient conversations. Some women arrive convinced that any hormone therapy will cause cancer. Others come in with social media information from prominent menopause physicians, ready to start immediately.
Both situations call for the same approach. Physicians must acknowledge current evidence, acknowledge the gaps in that evidence, and explain the monitoring plan.
Baby steps can help hesitant patients. Starting with oral micronized progesterone alone addresses sleep and anxiety. Once patients feel better, they’re often more open to adding estrogen.
The goal is a partnership built on listening to patient values, educating on evidence, and building a plan together.
Private Physicians Alliance members can access the full recording of this annual meeting session, including the Q&A on complex cases such as genetic clotting mutations and post-60 initiation. Learn more about membership to join the conversation.